- March 15, 2024
- Siddhi Talgaonkar
- Gestational and Neonatal
Postpartum Gut Health: A Guide for New Mothers
While new moms are filled with excitement and surprise at the birth of their child, the postpartum phase frequently causes a flurry of changes in their lives. It's a period of great physical and mental change, from enduring restless nights to getting used to the responsibilities of caring for a newborn. The effect postpartum recovery has on gut health is one area that is sometimes disregarded but has benefits if given careful consideration. Understanding and promoting gut health becomes essential for the long-term health of the mother as well as that of her child, as the body experiences extraordinary changes following childbirth.
Changes in a woman's body after the birth of a baby
During the postpartum period, a woman's body undergoes significant changes as it transitions from pregnancy to motherhood. Uterine involution, marked by the contraction and shedding of the uterine lining, occurs, along with hormonal fluctuations affecting mood, lactation, and gut diversity. Breast changes prepare for lactation, while vaginal changes like discharge and swelling are common. Side effects such as tiredness, mood shifts, and weight loss are experienced, alongside pelvic floor alterations and postpartum hair loss.
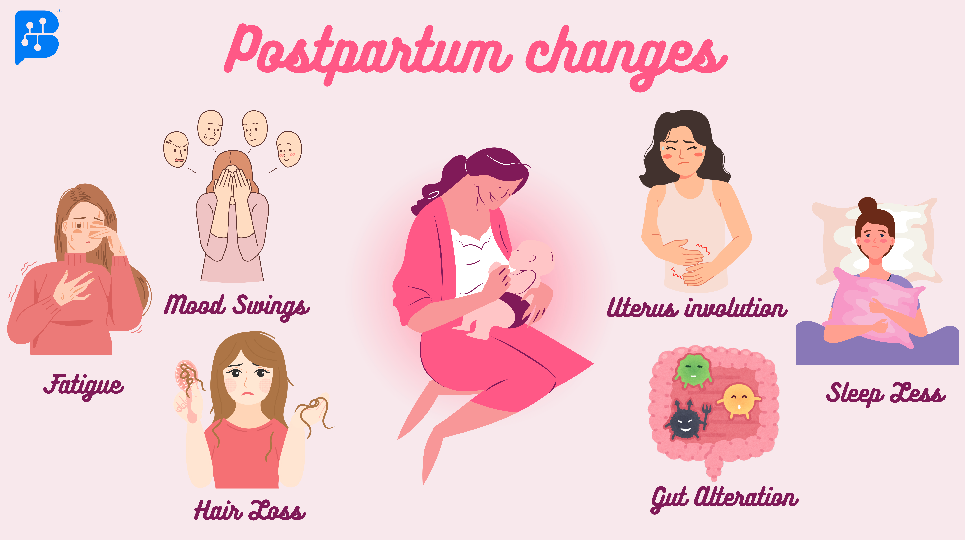
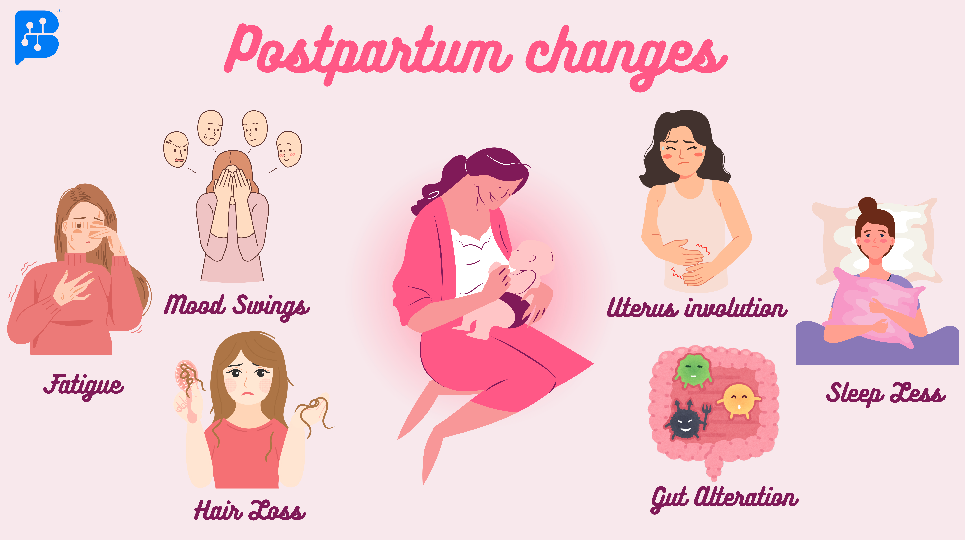
Postpartum Changes in Mother After Delivery
After giving birth, the woman experiences several physical and emotional changes. Constant mood fluctuations, exhaustion, lack of sleep at night, and hair loss. Numerous problems, including cramping, accompany uterine involution and gut alteration.
Understanding Postpartum Gut Health
1. Physical Changes and Gut Microbiota
Physical changes, including uterine involution, hormonal fluctuations, breast changes, and vaginal alterations, are accompanied by shifts in gut microbiota composition. These changes can affect gut motility, digestion, and overall gut health, often leading to symptoms like constipation or diarrhea.
2. Sleep disturbance and Gut Health
Sleep disruption and deprivation are major problems for women in the postpartum period as they balance the responsibilities of infant care. Getting enough sleep is essential for the immunological and neurological systems to operate properly and for the postpartum healing process. However, sleep disturbances are often linked to depression and exhaustion, which presents more difficulties for new moms. Long-term sleep disturbances can have profound effects on metabolism, hormone release, and the risk of cardiometabolic diseases, including diabetes and obesity. Research has revealed fascinating connections between sleep, circadian rhythm, chronic fatigue syndrome, and the gut microbiota.
Research has revealed that individuals suffering from chronic fatigue syndrome frequently display a less diverse gut microbiota, which can result in dysbiosis and heightened gut permeability. The disruption of the gut flora may worsen long-term inflammation and make it more difficult for new mothers to heal from childbirth.
3. Mental Health and Gut Health
Gut health and mental health problems, especially postpartum depression (PPD), are closely related throughout the postpartum period. Research has shown that changes in the variety and composition of the gut microbiome can affect the synthesis of neurotransmitters and other neuroactive substances, which can then affect the control of emotions and brain function. Additionally, it is becoming more widely acknowledged that a major role in mental health is played by the gut-brain axis, a bidirectional communication link between the gut and the brain.
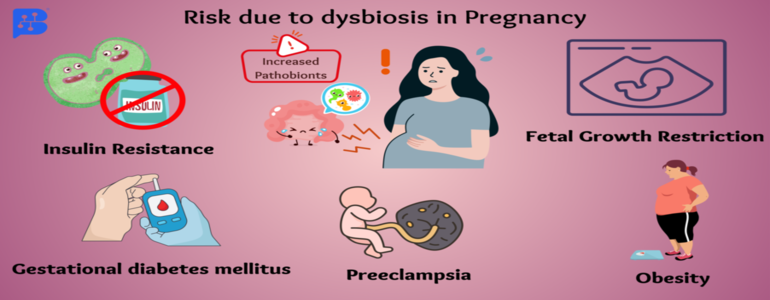
Disruptions in this axis, such as gut microbiota imbalances or increased intestinal permeability, may lead to the emergence or worsening of mental health issues, including postpartum depression. Furthermore, gut health and microbiome composition can be further influenced by hormonal changes that occur during pregnancy and the postpartum period, which may increase a person's vulnerability to mental health problems. In general, there is a complicated and varied association between gut health and mental health throughout the postpartum phase.
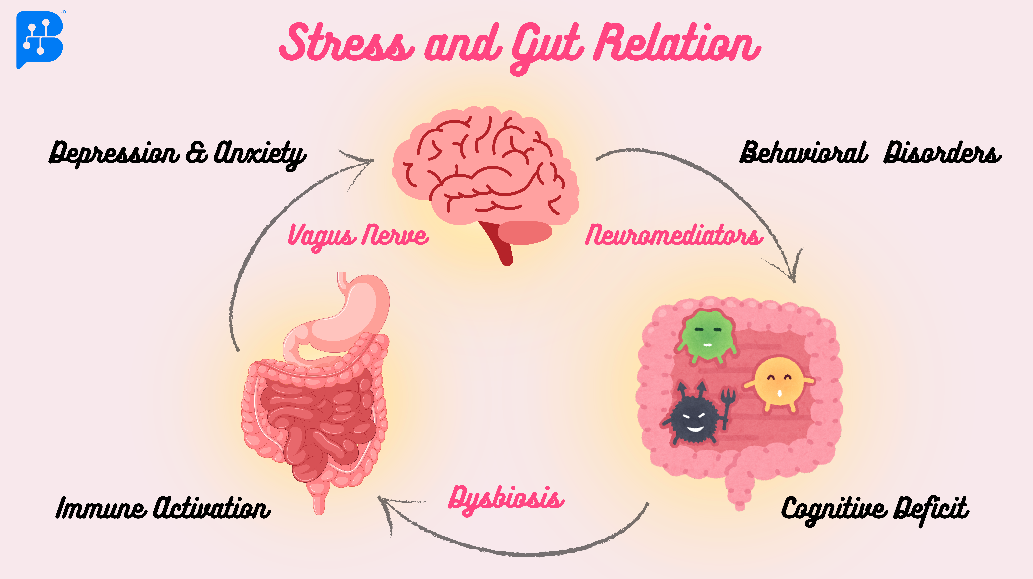
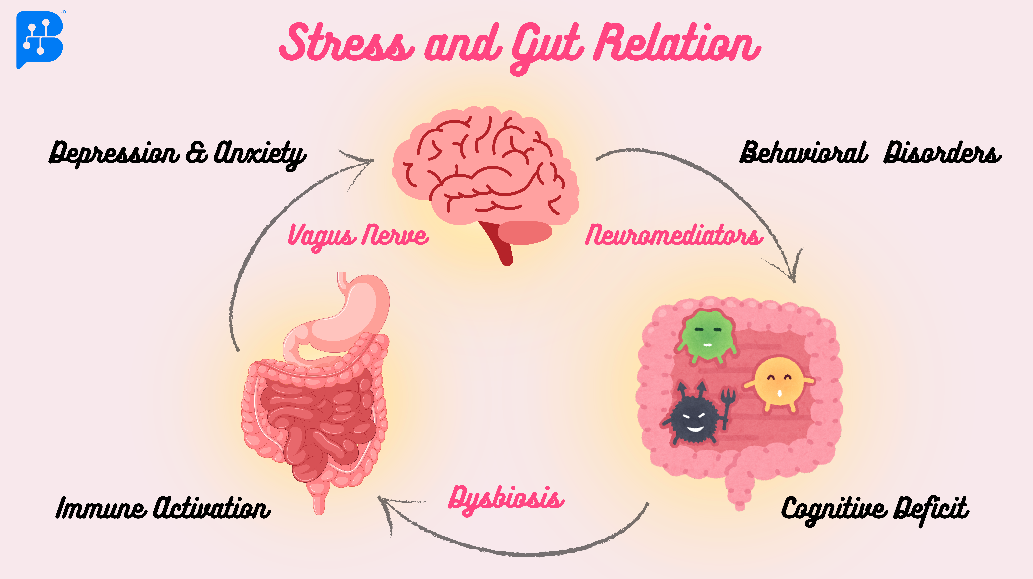
Image no. 2- Stress and Gut Relation
The gut and the brain talk to each other in many ways. One way is through the vagus nerve, which connects them directly. Another is through substances produced by the gut bacteria that can affect the immune system and the gut lining. Also, gut bacteria create chemicals called short-chain fatty acids (SCFAs) that can influence the brain. Additionally, cells lining the gut release hormones that can send signals to the brain. These signals control important functions like mood, inflammation, and stress response. When the gut bacteria get out of balance, causing dysbiosis, it can disrupt these signals and contribute to stress-related problems.
Digestive issues and gut health
Many women have digestive problems during the postpartum period, including bloating, constipation, and pain, which can have a serious negative effect on their health. These problems are frequently associated with modifications to gut health, such as adjustments to the makeup and functionality of the gut microbiota. The delicate balance of bacteria in the gut becomes disturbed during pregnancy and delivery, which can result in dysbiosis and digestive issues. These problems can be made worse by elements including dietary modifications, stress, hormone swings, and postpartum drugs.
Breast infection and gut health
Breast inflammation, or mastitis, can have several reasons and is most common in the postpartum phase. 3–33% of nursing mothers experience it, usually in the first few phases of lactation. A prominent explanation for bacterial mastitis is an overabundance of pathogenic strains in the mammary gland, such as group B streptococci and Staphylococcus spp. A series of immunological and metabolic alterations that result in the clinical signs and symptoms of mastitis are caused by this excess, disrupting the balance of beneficial bacteria. Unfortunately, the discomfort, fever, and malaise associated with mastitis frequently discourage breastfeeding. Misconceptions regarding the transmission of infection to the newborn while breastfeeding may also deter moms from nursing their babies while undergoing therapy.
Despite the challenges posed by these modifications, they are all integral aspects of the body's natural recovery and adaptation to the demands of motherhood.
How can you take care of your gut during postpartum?
Stay Hydrated: Maintaining gut health and preventing constipation may be achieved by drinking enough fluids, especially warm beverages, first thing in the morning. This also helps keep stools soft and encourages bowel movements.
Boost Dietary Fiber: Include naturally occurring dietary fiber sources in your diet, such as fruits, vegetables, nuts, almonds, and flaxseeds, to maintain a healthy colon by encouraging regularity and avoiding constipation.
Regular Exercise: Physical activity on a regular basis enhances gut health and digestive function by stimulating bowel movement and improving circulation. Walking and yoga are examples of gentle workouts that might be very helpful in the postpartum phase.
Consume Probiotics: Using probiotics to repopulate a healthy gut flora aids in optimal nutrient absorption and improves digestive health in general. Incorporating probiotics into the diet through foods like yogurt (curd), buttermilk (chaas), and fermented dishes like idli, dosa, or dhokla helps improve gut health in the postpartum phase.
Make Sleep a Priority: During the postpartum phase, good sleep is essential for gut health and general well-being. Improved sleep quality may be achieved by establishing a regular bedtime, creating a sleep-friendly atmosphere, and asking partners or family for assistance with nocturnal baby care.
Control Mental Stress: During the postpartum phase, gut health and general wellness depend on the control of mental stress. Techniques that can help lower stress and improve emotional well-being include mindfulness meditation, deep breathing exercises, and asking for help from loved ones or mental health specialists.
How can you enhance your baby’s gut health?
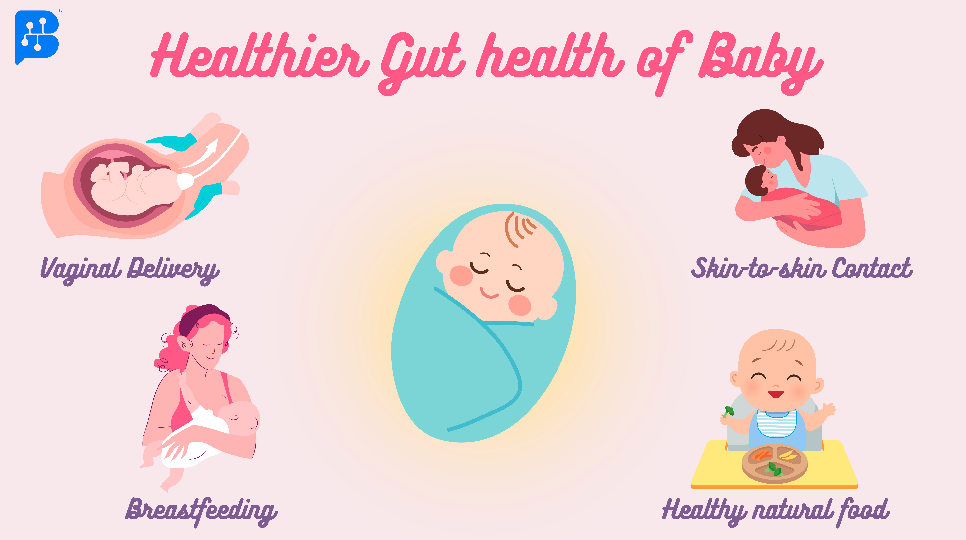
Throughout infancy and beyond, you should support the healthy development of your baby's microbiome. Vaginal birth introduces a broad range of microorganisms, encouraging the early development of the baby's microbiome. Breastfeeding encourages the development of a varied microbiome in your child by giving them vital nutrients and beneficial probiotics. If nursing isn't an option, you could choose to use screened milk from milk banks. In the first few weeks, embrace skin-to-skin contact and refrain from using harsh cleaning solutions to support your baby's developing microbiome and impart the advantages of your mature microbiota. Prioritize a diet high in whole, natural foods when your baby starts to eat solid meals to help the diversity and health of the microbiome.
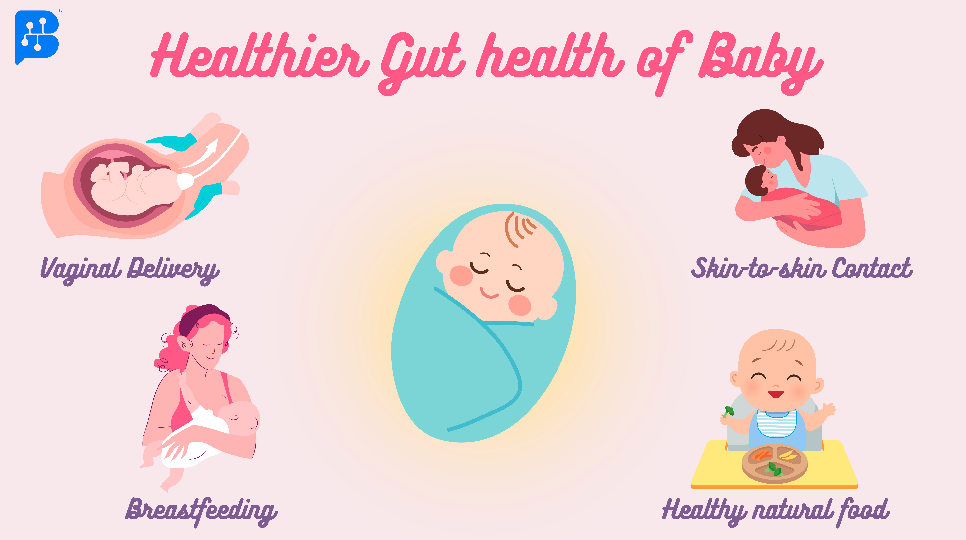
Image no.3- Healthier Gut Health Ways of Baby
The newborn baby is completely sterile when entering this world. So the first exposure to bacteria is during birth through the vagina. Breastfeeding and skin-to-skin contact, which involve a lot of hugs and kisses for the baby, help introduce mature microbiota. After some time, enhance the baby's diet with a probiotic-rich natural diet.
Conclusion
New moms experience a variety of physical and psychological changes throughout the postpartum phase. It's a period of major adjustment and adaptation, from the amazing changes in the body to the difficulties in managing sleep, emotional stress, and digestive concerns. Understanding the significance of gut health throughout this stage is critical since it affects both the mother's and her child's well-being. Women may maintain their gut health and go through the postpartum journey more easily and resiliently by placing a high priority on water, dietary fiber, exercise, probiotics, restful sleep, and mental stress management throughout their pregnancy and beyond.
Remember, dear moms, that in the middle of all the change and responsibility, taking care of yourself is just as crucial as caring for your child. You are strong and capable, and you deserve love and support as you embark on the amazing path of parenthood!
References
-
Weerasuriya, W., Saunders, J. E., Kis, L., Ho, T. T., Xu, K., Lemas, D. J., ... & Louis-Jacques, A. F. (2023). Maternal gut microbiota in the postpartum Period: A Systematic review. European Journal of Obstetrics & Gynecology and Reproductive Biology.
-
Mutic, A. D., Jordan, S., Edwards, S. M., Ferranti, E. P., Thul, T. A., & Yang, I. (2017). The postpartum maternal and newborn microbiomes. MCN: The American Journal of Maternal/Child Nursing, 42(6), 326-331.
-
https://www.biocodexmicrobiotainstitute.com/en/postpartum-depression-changes-gut-microbiota-under-spotlight
-
https://www.mothernutrient.com/blogs/mother-nutrient-blog/how-to-ease-common-postpartum-digestive-issues