- Feb. 11, 2019
- BugSpeaks
- Microbiome and Lifestyle
The role of Gut Microbiome in the Wellness World
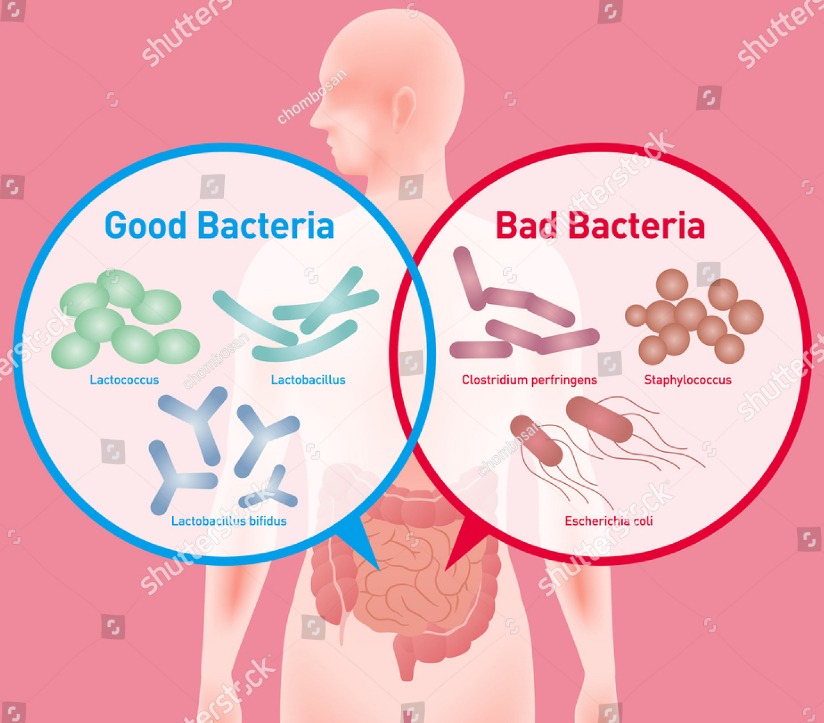
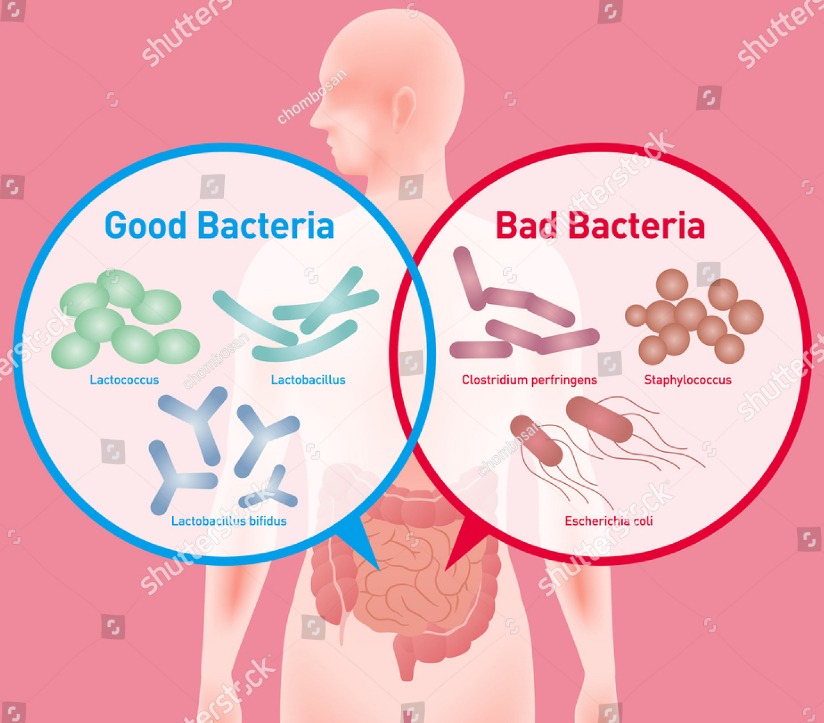
The indigenous microbial communities are represented as microbiota, while the collection of microorganisms in the host environment where they inhabit and their genomic contents is known as microbiome. Recent advancements have transformed clinicians’ ideas about the role of microorganisms in human health and diseases. Interestingly, it has been realized that the microbiota inhabiting in our body provides a necessary ecosystem for mutual benefits, such as improving the digestion process, protection against pathogens, bioconversion of nutrients, etc. It has been reported that several trillions of microbial cells occupy different parts of the human body. Our body constitutes more bacterial cells than human cells, and they considerably affect our day-to-day lives. Therefore, the microbiome influence on human diseases and vice versa can be wide-ranging. For instance, the gut microbiota can modulate the functions of the gastrointestinal tract, produce chemicals, improve immune functions and even control the behavior. Likewise, a chronic lung disease may modify the composition of lung microbiome, and successively impact on immunity and host defense, leading to additional exacerbations of diseases. Also, bacteria, such as Lactobacillus, Bacteroides and Bifidobacterium synthesize secondary bile acids, which are crucial for the lipid transport. As a beneficial bacteria,Bifidobacterium generates Vitamins (B12, K, biotin, thiamine). The microbial diversity is very high in the gut region as compared to any other body parts (the skin, gums, and vaginal sites). Hence, most of the current investigations are focused on the gut microbiome and its significant role in establishing good health. The gut microbiome varies from one person to another, though they have some common illnesses like Obesity, Type 2 Diabetes or Inflammatory Bowel Disease.
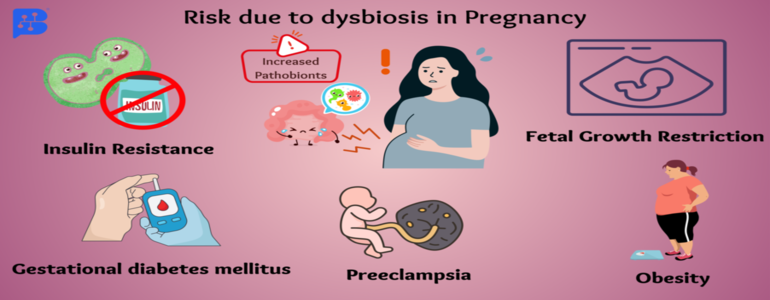
A disease can be anticipated with the loss of helpful functions by the gut microbiome or by invading microbes in the gut. In other words, a disturbed gut microbiome leads to several diseases, particularly which are allied with our lifestyle aspects. Investigations have proved the connection between these microbes in our gut and many chronic disorders, such as Obesity, Diabetes, Coronary Artery Disease, Parkinson’s, Alzheimer’s, Lupus, Psoriasis, Autism, etc. Therefore, a proper nourishment of our gut microbiota can restore health conditions and make us feel happy. The consumption of healthy diet included with prebiotics and probiotics, avoiding antibiotics intake unless very obligatory, and a regular exercise may be helpful in improving our gut microbiota. In humans, the gut microbiome has co-evolved with its host since from ages and, hence, it performs a variety of crucial activities in the host, including digestion, nutrition, detoxification, body defense, improving immunity, and disease mediation. Accordingly, the human gut inhabits a wide range of microbes with high species diversity, with most of them being Bacteroidetes and Firmicutes.
The occurrence of harmful bacteria in our gut may cause a leaky gut syndrome, which happens due to the high permeability of the intestinal walls, causing leakage of undigested food particles, bacteria, and many other substances into the nearby tissues. The leaky gut syndrome is directly connected with several health problems, such as chronic fatigue, Stomach aches, Insomnia, Inflammatory Bowel Syndrome, Constipation, Diarrhea, Headaches, Depression, Cardiac problems, Pancreatic illness, etc. Our brain is directly connected to the gut microbiome, which is known to have a role in controlling or regulating our body functions. It may act autonomously (as another brain), or in combination with the brain. Hence, an unbalanced gut microbiota may trigger variations in our mood and behavior. Some of the neurological problems, such as Depression, Anxiety, Autism, and anger are correlated with health conditions of gut microbiome. A healthy microbiome can defend disease causing microbes in the body because, the beneficial microbes secrete substances or create the detrimental environment that can resist the growth of pathogens or even destroy them. For instance, volatile fatty acids, and its other byproducts produced by healthy gut microbes prevent the survival of fungi and yeast. Likewise, the pH in the digestive tract is also balanced by the microbiome so that many toxic bacteria like Shigella, E. coli, and Salmonella cannot survive in that condition. These bacteria are known to cause intestinal diseases, Diarrhea, and Food poisoning.
Following good practices and lifestyle habits can keep our gut microbiota healthy, which in turn can impact on a healthy life. The conservation of a varied and prospering beneficial gut microbial population helps in keeping away harmful bacteria due to higher competition for the same nutrients and colonization sites. A diet, particularly rich in fibers is highly advised to maintain a healthy gut microbiota population. In addition, certain Prebiotics and Probiotic foods, such as Yogurt, Kefir, Cottage Cheese, Natto, Tempeh, etc., will certainly enhance our gut microbiota population and health. However, some of the bad lifestyle habits need to be avoided as they destroy both good microbiome and their diversity. It is suggested to avoid these bad habits such as, overuse of antibiotics, antacids, laxatives, and painkillers; drinking chlorinated water, eating sterilized foods or foods with altered fats; high intake of carbohydrates to name a few.
Molecular technologies, such as 16S ribosomal RNA sequencing, Microbiomics, Metatranscriptomics, Metaproteomics, and Metabolomics analysis have impressively improved our knowledge of the diversity, complexity, and functions of the gut microbiome within and between individuals. These high throughput technologies have delivered us with the capability to gain insights into the genes being expressed vigorously in the complex microbial communities. It has enabled us to elucidate the functional changes in directing the microbiome functions at specific environments, its interactions with the host, and functional changes involved in translating a healthy microbiome in the direction of a disease-driving configuration. Thus, the gut microbiome genomic analysis can provide a clue to the role of the gut microbiota and its impact on our health.
The analysis of different genes expressed by microbes in the gut facilitates us to identify the types of metabolites that they will produce. It helps in determining the microbiome role in our body. However, just getting a data may not be useful. We have to understand about the type of genes expressed, the levels of metabolites produced and their functions, and how to improve them through a defined diet, supplementations, or modifying lifestyle activities to improve the gut microbiota of an individual. Overall, this is a personalized medicine approach to help patients to improve their gut microbiome health to overcome many diseases. It will help us to precisely decide what, how and when to take right food in order to develop wellness in a short time. Based on the microbiomics data, a patient can be accurately treated with a proper diet and lifestyle modifications. In specific, this Gut microbiome test will help us to know about the absence of beneficial bacteria and good metabolites in our gut, and the need of probiotics, carbs, proteins, and fats or nutritional endorsements to restore good health in a personalized way.