- Dec. 2, 2019
- BugSpeaks
- Microbiome and Disease
From Gut to Joints: Microbiome & Arthritis
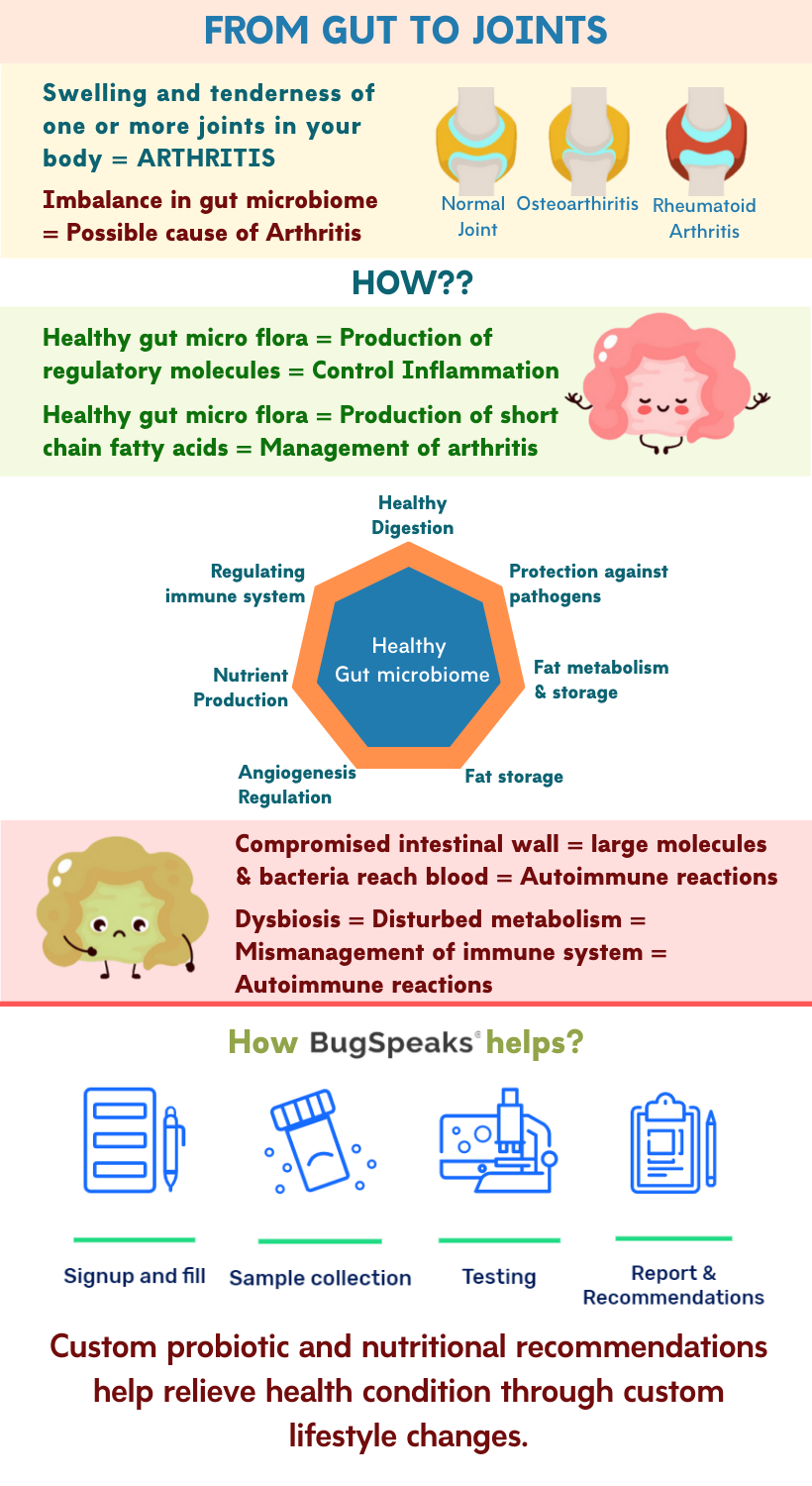
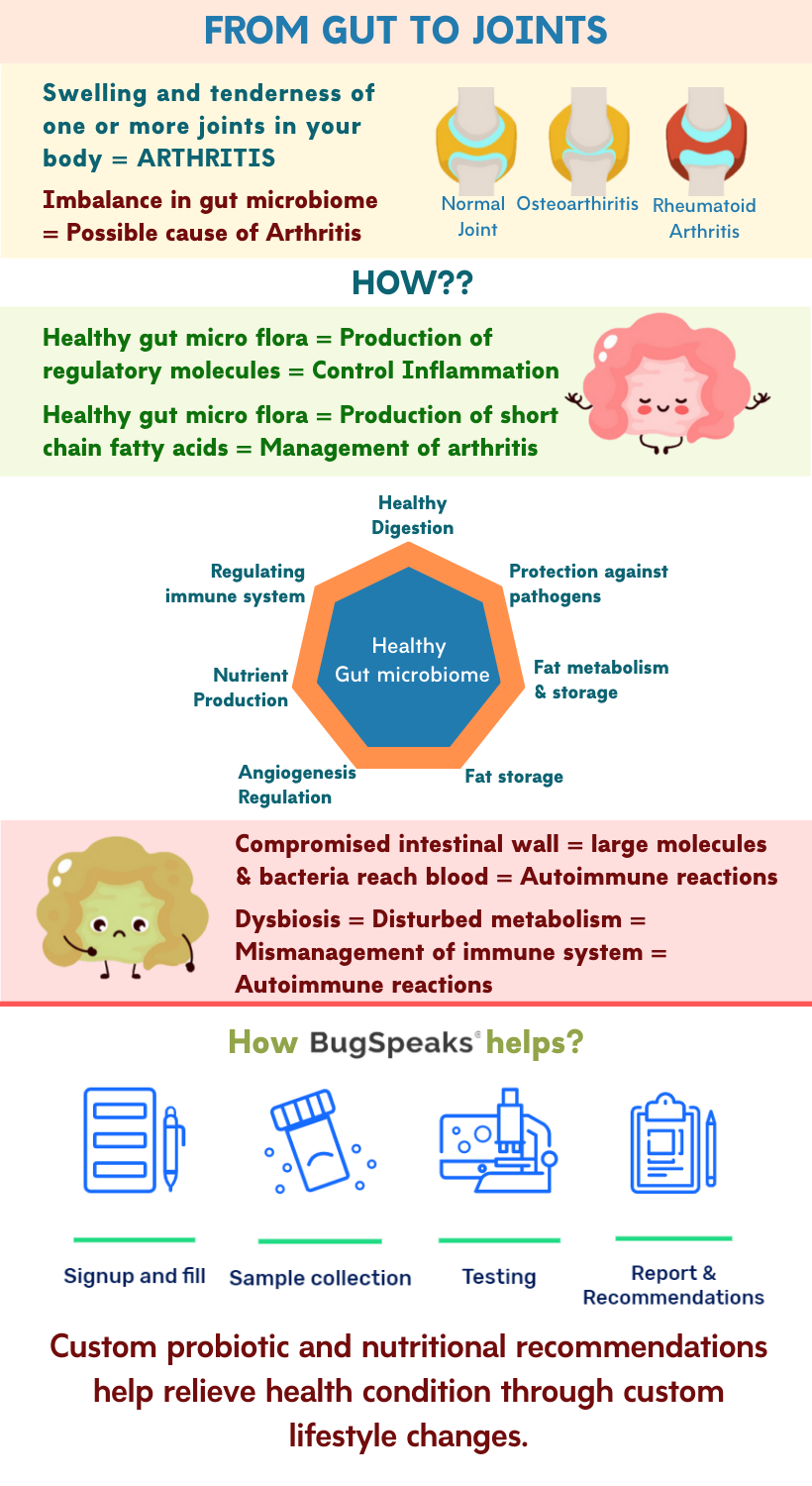
Arthritis is swelling and tenderness of one or more joints in your body. This disease is widespread, yet, not well understood. From the 100 different types of arthritis, osteoarthritis and rheumatoid arthritis represent the most common ones. Regardless of the type, symptoms are similar in all the cases, which include joint pain and stiffness. The symptoms typically worsen with age. However, people of all ages, sexes, and races have arthritis, with more prevalence in women. Being the leading cause of disability in the world, arthritis, often compromises quality of life.
Moreover, upon affecting weight-bearing joints, arthritis restricts one from walking comfortably or even sitting up straight. Per the treatment a doctor often advises medications, physical therapy, weight loss and exercise. But a diet alteration to transform your gut microbiome forms a rare recommendation. However, experts at world-renowned mainstream institutions nowadays acknowledge the role of the gut microbiome in certain types of arthritis, autoimmune arthritis. Autoimmune arthritis further includes rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis.
Few pieces of evidence:
Scientists have observed the digestive tracts of people with rheumatoid arthritis to be overpopulated with potentially disease-causing bacteria. Microbes like Prevotella copri, Collinsella sp., and Eggerthella lenta occur in high numbers while the number of healthy bacteria, like, Bifidobacterium, the Porphyromonas-Prevotella group of bacteria, Bacteroides fragilis subgroup, Eubacterium rectale, and Clostridium coccoides group is relatively low.
Also, people carrying the HLA B27 gene show a higher risk of developing autoimmune arthritis. This gene presents an association with changes in the gut microbiome. Thus, it presents a link between gut flora and rheumatoid arthritis and other forms of autoimmune arthritis.
Gut microbiome and autoimmune arthritis
Our gastrointestinal tract is home to a large and complex community of micro-organisms. This gut microbiota keeps our body fit in many ways. These include healthy digestion, production of nutrients, detoxification, fat metabolism and storage, angiogenesis regulation, protection against pathogens, and regulation of the immune system. However, overtime, under the influence of altered food habits, lifestyle, and medication (antibiotics and steroids) intake it undergoes modification. These alterations frequently lead to the imbalance of the intestinal microbiome. An imbalance in the gut microbiome can lead to chronic inflammatory and autoimmune diseases, such as arthritis.
Leaky Gut Syndrome and Arthritis
As per researchers and clinicians ‘Leaky Gut Syndrome,’ characterized with increased intestinal permeability also plays a role in arthritis. The syndrome results from the damage to the small intestine wall. When healthy, the small intestine only allows useful nutrients to pass across and enter the bloodstream. However, upon damage, the intestine permeability stands compromised and larger molecules like half-digested fats, proteins, starches, and even bacteria reach the blood. These microbes are often gram-negative gut bacteria whose outer membranes contain molecules called lipopolysaccharides. The body recognizes lipopolysaccharides and partially digested food products as foreign substances, and they trigger an immune response. The antibodies thus produced, travel through the bloodstream and create an inflammatory response in other parts of the body, including joints, leading to arthritic pain and swelling. Though the matter is controversial, yet there is evidence that shows that healing a leaky gut with a strict diet and nutritional supplements can help to control arthritis.
Inflammation and Arthritis
Inflammation is a common feature in almost all types of arthritis such as rheumatoid arthritis, gout, ankylosing spondylitis, psoriatic arthritis, and pseudogout. Even osteoarthritis—which, lacks an autoimmune response— may present with inflammation. A healthy gut microbiota find implication in inflammation control by influencing the differentiation of inflammatory cell types, and production of regulatory molecules, like cytokines.
A healthy gut means a healthy body
These days correlation between intestinal health and the gut microbiome remains well-understood. So, the best way to deal with arthritis is to maintain a healthy diet to have a healthy gut flora. Diet alteration stands as a great way to achieve this but offers temporary and quick shift in the gut microbiome. To instil a permanent shift toward healthy gut flora a long-term commitment to a healthy diet full of leafy vegetables and plant-based whole foods remains essential. A fibre-rich diet helps beneficial gut flora to flourish. They produce short-chain fatty acids from fibre present in foods.
These short-chain fatty acids contribute to the wellbeing of the intestinal lining and may prevent disease. Moreover, short-chain fatty acids help curb glycaemic response and satiety, promote weight loss, enhance mineral absorption, and reduce systemic inflammation. All of these are important for the management of arthritis. These changes can lead to a better functioning immune system, reduce inflammation, and lower arthritis-related pain. On the other hand, the bacteria thriving on a high-protein, low-fibre diet produces ammonia and other compounds, having potentially harmful effects. Therefore, a healthy, balanced gut microbiome fosters healthy intestines, and vice versa, both of which play a crucial role in a person’s overall health.
Other factors
In addition to diet, other factors, including heredity, stress, and the environment also influence the gut microbiome. For this reason, regular exercise, meditation, and reduction in exposure to toxins must accompany gut rehabilitation through a healthy diet. Physical exercise also alters the composition and functional capacity of the gut microbiota, independent of diet. However, exercise-induced alterations of gut microbiota may depend on obesity status, exercise modality, and exercise intensity.
Get ‘Gut Microbiome Test’
As we all have a unique set of gut-microbiota, the dietary recommendations must be tailor-made. So, if you want to fix your arthritis before it gets worse, take a ‘Gut Microbiome Test.’ This test uses cutting edge DNA sequencing technology in patient stool samples to map and identify the unique array of micro-organisms present in the gut. Then this data is used to provide a customized dietary recommendation consisting of probiotics and prebiotics. This diet is targeted at the improvement of arthritis. As it may take quite a few months to get your intestinal flora changed, you are advised to follow the diet plan religiously for several months before deciding whether it works or not. Patience is the key to succeed through gradual progress.