- Feb. 20, 2020
- BugSpeaks
- Microbiome and Disease
Ulcerative colitis: Multiple issues of Dysbiosis
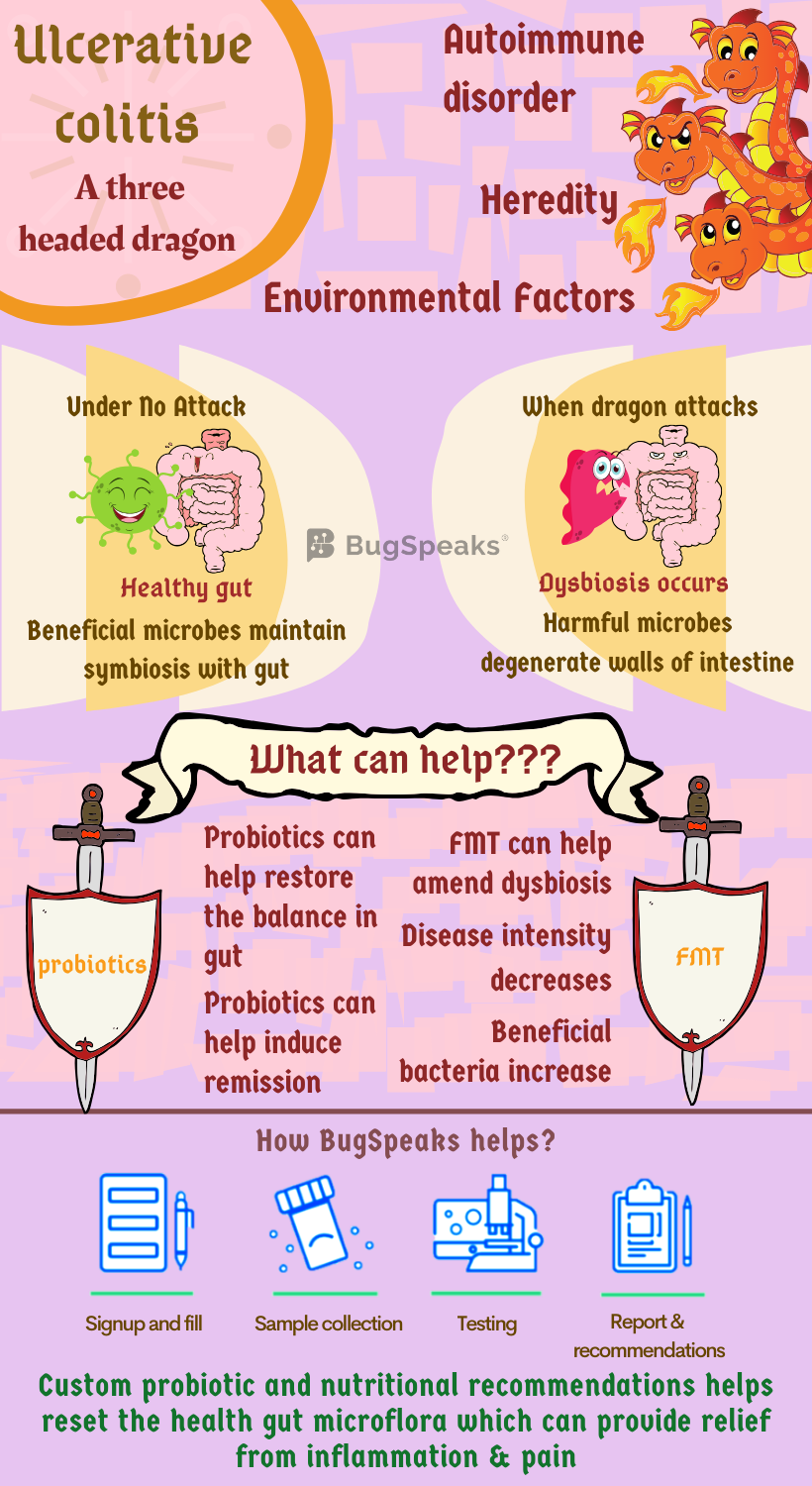
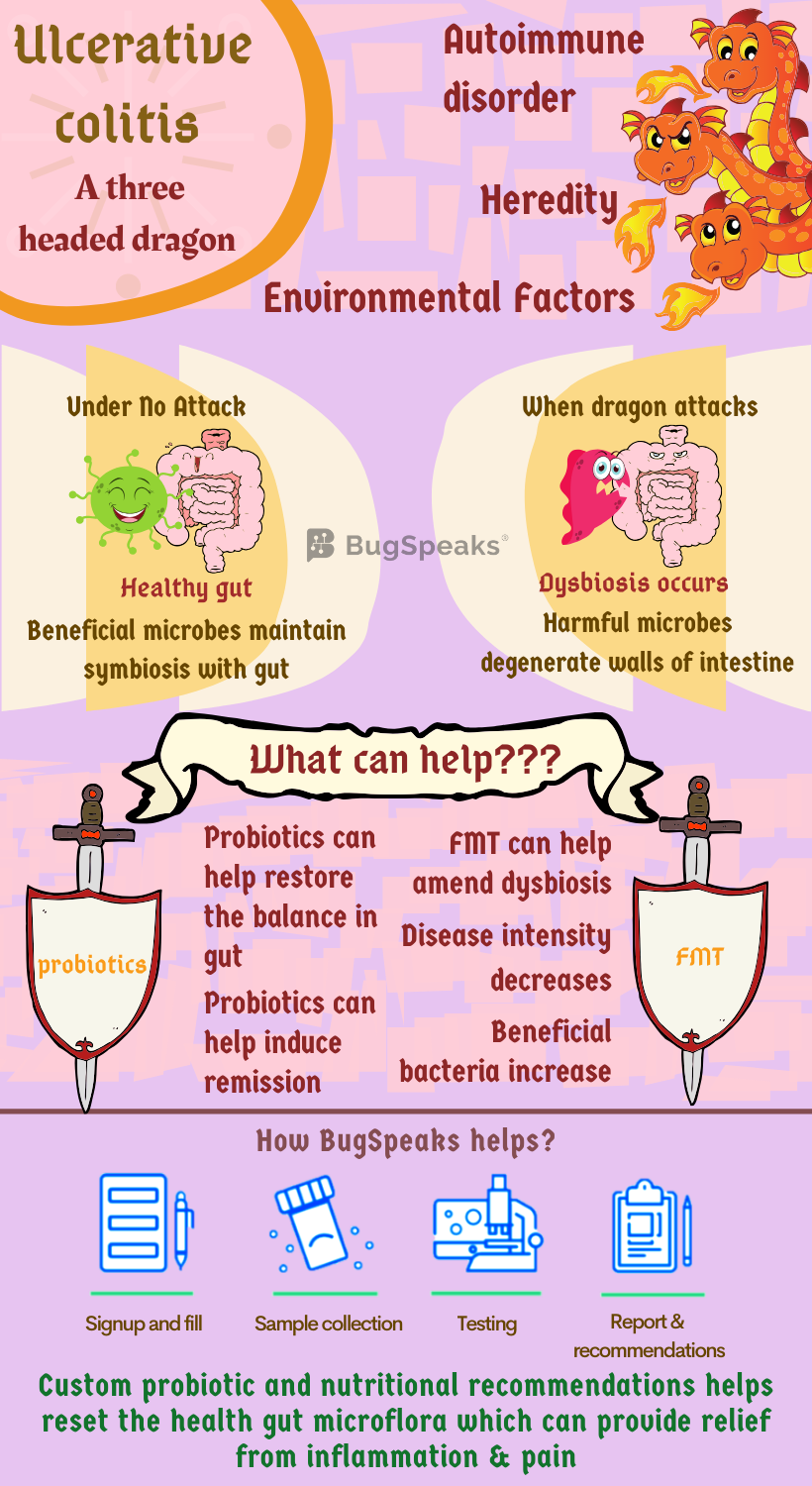
A common understanding of probable disease-causing mechanisms places diseases as genetic, autoimmune, or/and acquired due to the environment. But what if a condition can affect you through any of the three mechanisms. Well, that would be threatening. Such is the story plot of Ulcerative colitis (UC). A life-long illness, which affects the innermost lining of the lower part of the digestive tract, colon, and rectum. Think of ulcerative colitis as a three-headed dragon. It can exhale upon you the fire of ulcerative colitis through heredity, an autoimmune disorder, or environmental factor.
You don't get reduced to ashes but indeed suffer from symptoms like diarrhoea, often accompanied by blood or pus, bowel pain and cramping, rectal bleeding, bloody stool, the urgency to defecate. Consequently, you can lose considerable weight. Generally, the symptoms develop over time, and they differ depending on the location of the inflammation. The type and severity of the symptoms vary from person to person. Though rare, at extreme conditions, UC can be debilitating and can sometimes lead to life-threatening complications.
Gut microbiome: your secret power
Which head of UC dragon gets you depends on how you conduct your life. UC finds close association with the complex ecological system of different candidate microbes residing in our gut. The dominant anaerobic bacteria in the gut form a sort of biofilm over deep-lying tissues. Consequently, they play critical roles in nutrition, permeability, and immune regulation. This group of bacteria, e.g., Bifidobacterium, Bacteroides, and Peptococcus, exist in symbiotic relation with us. Other members of our gut are conditional pathogens, e.g., Enterococcus and Enterobacter.
They maintain harmonious relations with the gut of a healthy individual who has ecologically balanced gut flora. But, if you don't take care, this small group of bacteria can become quite detrimental and can damage the gut. The third category contains mostly pathogens, e.g., Proteus and Pseudomonas. In an ecologically balanced gut, these harmful bacteria stay under check. However, hampering of balance due to any external or internal disturbances accentuates the harmful pathogens. They overpopulate and replace the physiological bacteria and resulting in disease development.
Keep the Ulcerative colitis dragon tamed
A symbiosis between us and gut microbes promote stability in intestine by inhibiting the colonization of pathogens. Our gut flora under normal circumstances maintains the inner layer of our intestinal tract to keep a relatively low level of inflammation. It helps our gut immune system to continuously screen and eradicate the detrimental microbes.
Moreover, the short-chain fatty acids (SCFAs) released by certain healthy gut bacteria, Faecalibacterium prausnitzii, and Roseburia, have several beneficial effects. They are the primary energy source of intestinal cells and also acts as potent modulators of immune response. Additionally, they also suppress tumours and act as neuroendocrine modulators of the intestine. However, the most significant function of SCFAs comprises of control over anti-inflammatory genes involved in gut immunity.
Thus, gut dysbiosis, which results in a loss of diversity of intestinal microbiota, influences UC. In UC, dysbiosis, by approximately 25% as compared with that of healthy controls, results in an invasion of pathogenic bacteria in the intestinal mucosa. Some common gut bacteria, Akkermansia muciniphila, and Roseburia lessen whereas detrimental ones, Mycobacterium avium paratuberculosis, adherent-invasive Escherichia coli, Clostridium difficile, Helicobacter species11, Salmonella species, Yersinia, Fusobacterium, Norovirus, and Listeria16 increase in UC.
These gut damaging bacteria secrete certain toxic elements, which makes the intestinal wall more porous. Furthermore, the enhanced synthesis and secretion of immunosuppressive factors lead to the degeneration of intestinal physiology. All of these ultimately results in immune dysfunction and damaged intestinal epithelial cells. All this amplifies gut inflammation. So, care for autoimmune reactions and environmental factors by keeping stress at bay and eating healthy fibres is necessary.
Probiotics: Your knight in shining armour?
Gut friendly bacteria in the live state are known as probiotics. Relevant candidates of this group are Lactobacillus, Bifidobacterium, and Enterococcus. They play several essential functions in gut physiology. Firstly, they compete with pathogens for adhesion sites and nutrients and replaces the harmful ones, while, they correct the intestinal microbial imbalance. Additionally, they maintain and restore complete intestinal mucosal barrier function. Fourthly, they promote immune tolerance by secretion of anti-inflammatory factors of the intestinal mucosa and thus inhibit pathogenesis. Fifthly, they help to mend the intestinal and total immunity of the body. And lastly, they prevent cell death of intestinal mucosa. Thus, probiotics can effectively induce and maintain at-least temporary remission in UC patients.
However, some studies associated with probiotics and UC present contradictory results. They have demonstrated that treatment with probiotics amplified bowel movement, resulting in frequent defaecation and diarrhoea like symptoms. Other studies show that probiotics such as Lactobacillus acidophilus LA-5 and Bifidobacterium showed no difference between UC remission patients and the control group20. Better study design with bigger study group based clinical trials, therefore, remains desirable to establish the exact role of probiotics in UC management.
Faecal Microbiota Transplant: Helping the damsel in distress
Faecal microbiota transplantation (FMT) remains another healthy option for slaying UC. The transplant of faecal bacteria from a healthy donor to a recipient, suffering from UC, can quickly resume the normal function and composition of intestinal microbiota. Don't worry. No one will make you eat the poop. In this process, freshly collected faeces are dissolved and homogenized in saline or water, filtered and transplanted within 6 to 8 hours of collection. After FMT, the microbial diversity in the receivers' gut became very much similar to that of the donors.
FMT is a simple procedure and can be done with ease. This is also a rather safe mode of treatment. Interestingly, according to some reports, repeated FMT might be better than single transplantation. As, after several years of treatment, there is a chance of microbial reversal. Thus, it is vital to undergo FMT again after several years. However, the number of procedure and gap between two transplantations need to be evaluated depending on the personal diversity in every case.
The proportion of beneficial bacteria and diversity increases and thus amending dysbiosis. This blend of beneficial bacteria often contains SFCA producing ones, which improve intestinal ecology and permeability of the mucosal wall — thereby lowering the disease intensity. The proportion of Lachnospiraceae, a butyrate-producing bacterium, gets amplified by FMT. It suggests Lachnospiraceae as the vital bacteria in the success of FMT.
Adverse reactions of gut flora
Complications of FMT are rare but can be dangerous and life-threatening. The complications include abnormally low blood pressure, norovirus infection, perforation of the colon, pneumonia, cytomegalovirus infection, bacteraemia, and others, are just a few among many others. For these reasons, to be on the safe side, long-term follow-up remains essential for patients undergoing FMT.
Gut microbiome test: A personalized armour against UC
UC and gut flora are interlinked. To have an idea of the harbouring microbes in our digestive tract, a 'Gut Microbiome Test' is essential. Cutting-edge' DNA sequencing technology' helps to detect the exclusive range of micro-organisms in patient stool samples. Based on this result, a tailor-made, therapy, and diet are prescribed for every individual. Although a complete treatment of UC remains elusive, highly effective management remains a possibility. With proper treatment, the severity of the disease can be managed up to a large extent. Most people with UC attain long-lasting remission and a hassle-free life with appropriate therapy and lifestyle.