- Feb. 27, 2020
- BugSpeaks
- Microbiome and Lifestyle
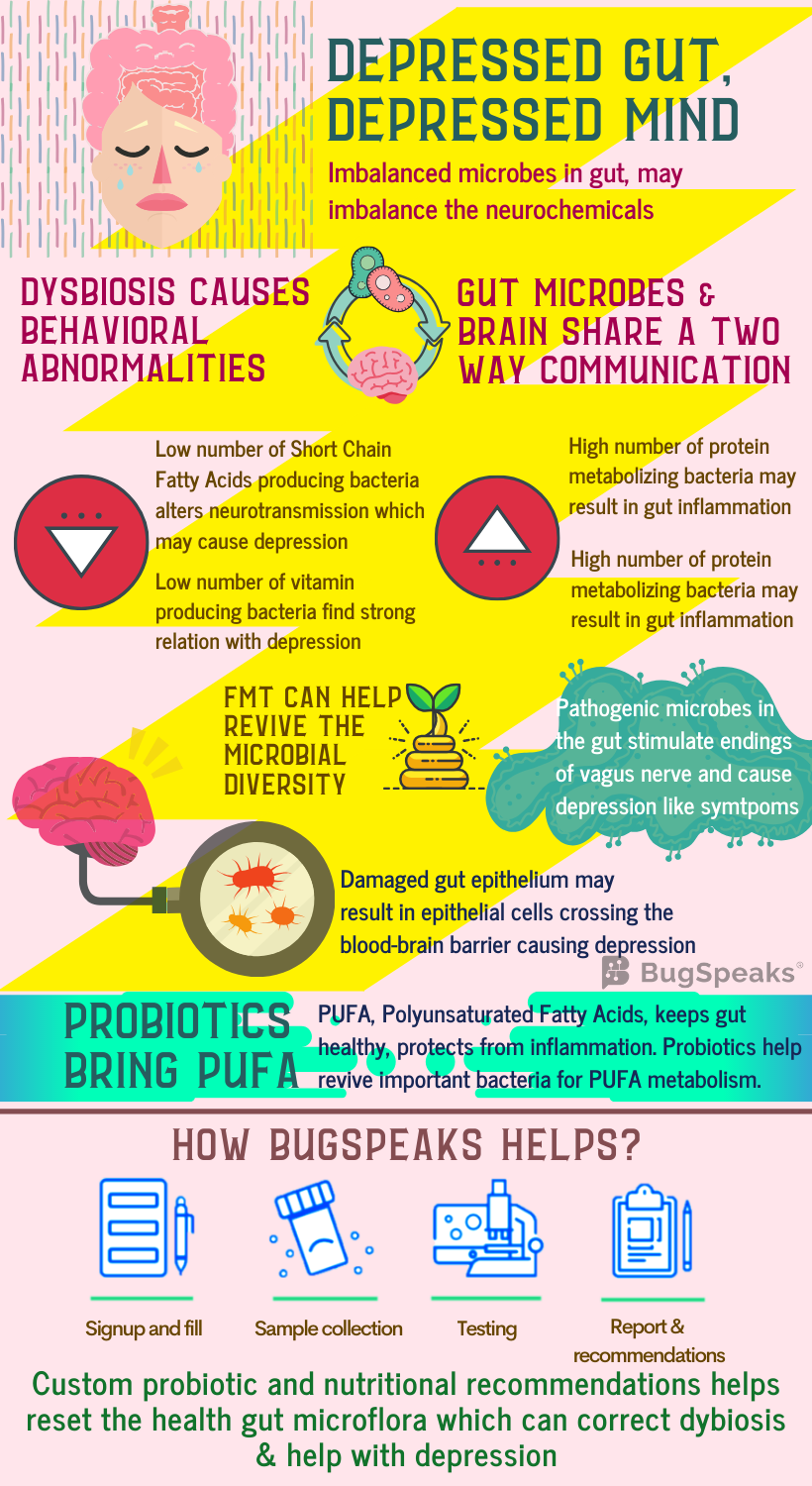
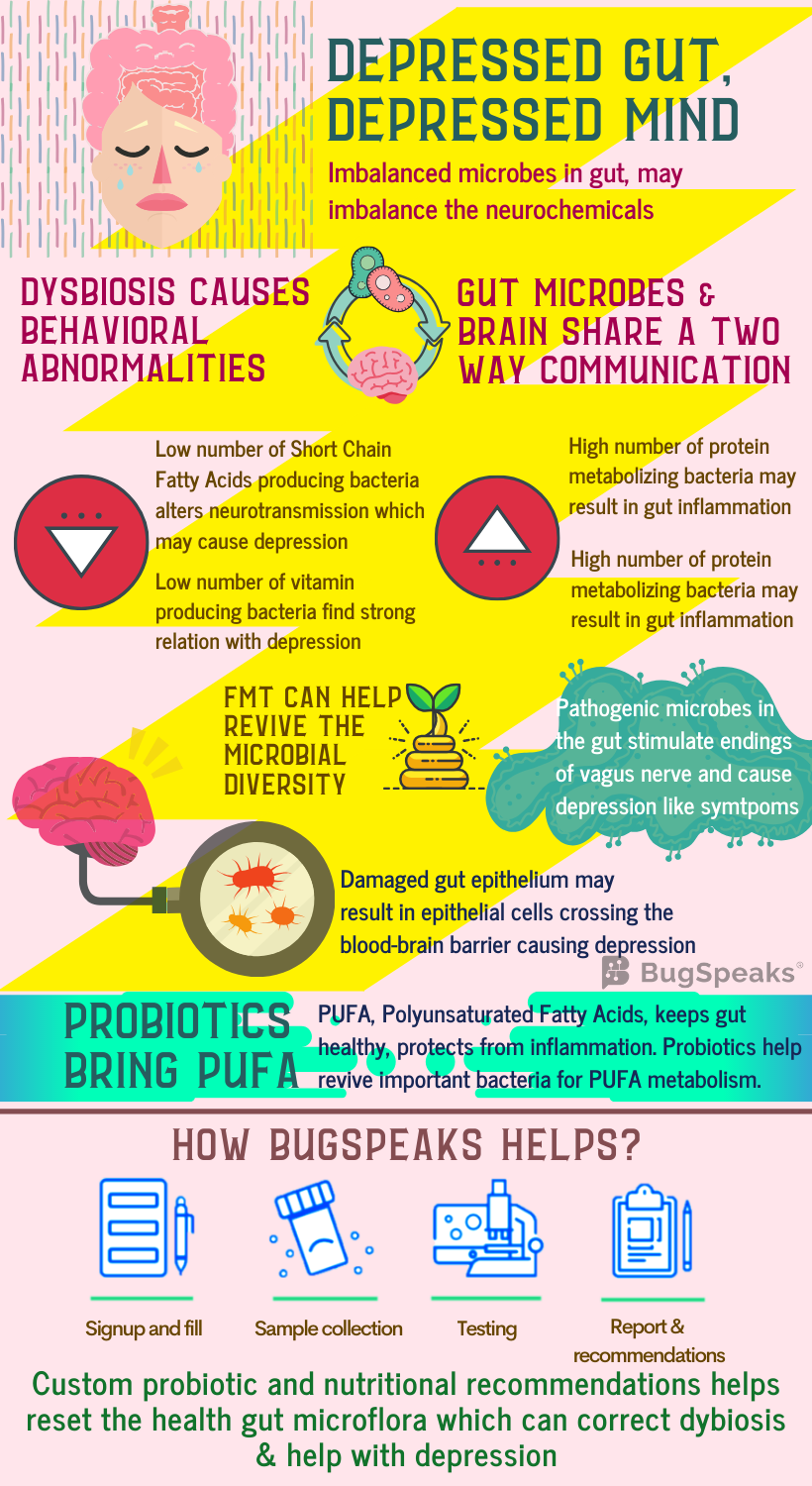
Depressed gut, Depressed mind
We all might have experienced bouts of depression some time in our life. Depression, a common psychiatric illness, presents a demoralized state wherein both the mind frame and body get affected. It affects feelings and judgmental capabilities and compromises the quality of life. Usually, depressed people are unable to concentrate and feel low all the time. Consequently, their performance in different areas such as academics or profession drops, causing additional stress. In extreme cases, it may lead to severe hopelessness and self-harm, with the thought of self-destruction and death.
Depression, stress, and anxiety all are interrelated and characterized by alteration in food habits and sleeping patterns. Stress and depression influence the release of cortisol (stress hormone). Cortisol modifies gut immunity, ultimately altering the microbial population in gut. It causes a significant modification in the gut microbial diversity, in terms of intensification or decline of individual species. However, the introduction of different genera or the complete removal of specific bacterial genera is not observed.
Role of Gut Microbiome
The gut flora of clinically depressed individuals differs in terms of the abundance and diversity of the common microbes. These include Bacteroidetes, Firmicutes, Proteobacteria, and Actinobacteria. Further, a reduced abundance of bacteria metabolizing carbohydrates also occurs in individuals with depression as compared to healthy ones. These include Bifidobacterium, Faecalibacterium, Bacteroides Coprococcus, Dialister, and Ruminococcus. While several other bacterial species, playing a pivotal role in protein and amino acid metabolism, remain over-populated in depressed subjects. Such bacteria involve Clostridium, Klebsiella, Parabacteroides, Streptococcus, Oscillibacter, and Alistipes.
Dysbiosis
Depression and gut dysbiosis find a deep connection as the gut and brain share a two-way communication. The reduced richness and assortment of the vast array of the microbes in our gastrointestinal tract also influence our mind frame and mood swings. Such correlation has been indicated by a small number of studies where dysbiosis found a relation with abnormalities in behaviour observed in neurodevelopmental disorders.
Production of Neurotransmitters
Apart from digesting and fermenting food and producing vitamins, gut flora also acts as a source of neurotransmitters, like, serotonin, gamma-aminobutyric acid (GABA), glutamate, dopamine, and noradrenalin. These metabolites play an essential role in maintaining gut immunity and prevent the colonization of the gut by pathogens. Reduction in levels of serotonin, noradrenaline, dopamine and malfunction of the glutamate-GABA system, find a close connection with depression and changed gut biology. Moreover, GABA producing, Bifidobacterium, also occur in a low number in depression.
On the other hand, environmental factors, the well-being of gut and relative diversity of gut microbes actively modify microbes which regulate neurotransmitter levels. Another neurotransmitter serotonin and tryptophan metabolites if unused, enter the circulation and influence behavioural responses. The gut microbiota also modifies brain function indirectly through changes in inflammatory states and immune status of the gut.
Carbohydrate metabolism
Edible fibers found in cereals, fruits, vegetables, nuts, lentils and grains are indigestible. Our gut bacteria convert the long edible fibers to short chain fatty acids (SCFAs). These SCFAs play an essential role in gut biology by acting as an energy source for intestinal cells and the microbes in gut. Interestingly the SCFAs inhibit enzymes which function as immunosuppressive, anti-inflammatory, and anti-depressive agents. Resultantly, low amounts of SCFA contributes to poorer energy and altered neurotransmission, resulting in depression. The SCFAs produced by the gut-friendly bacteria often pass in the systemic circulation and cross the blood-brain barrier through specific transport and enter into the brain. These SCFAs generate neurotransmitters and offers neuroprotection and acting as natural antidepressants.
Protein and Vitamin metabolism
Other than carbohydrate metabolism, gut flora also take part in protein and amino acid metabolism through fermentation or putrefaction. However, excessive intake of proteins can result in excessive production of toxic products such as ammonia, putrescine, and phenol, which contribute to stress and depression. Also, dysbiosis, causing low carbohydrate metabolism and high protein metabolism, find an association with intestinal inflammation leading to anxiety and depression.
Gut bacteria like Bifidobacterium, which synthesize vitamins like riboflavin, niacin, and folate, occur in a low number in depressed individuals. Low folate and thiamine find a strong association with depression and an inverse association with symptom severity.
Depression and Dysbiosis
On the other hand, it is reasonable to believe that depression leads to digestive problems and dysbiosis due to unhealthy eating habits or sleep-timings. Decreased ability to digest proteins causes accumulation of residual protein in the colon, aiding the growth of microbes feeding on them. This ultimately leads to elevated putrefaction and gut inflammation.
Several disorders linked with dysbiosis, like, irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), also find a relation with depression. Overpopulation of pathogenic bacteria causes gut inflammation, damages the gut epithelium and compromises intestinal wall permeability. In severe cases, the bacteria or the intestinal epithelial cells cross the blood-brain barrier, ultimately resulting in anxiety, depression, and related disorders.
Often activation of the Vagus nerve, controlling digestion, takes responsibility for regulating both dysbiosis and our mental health. Pathogenic microbes in gut flora influence vagal nerve endings distributed in the intestine, causing subsequent pathologic changes in CNS, and propagate depression-like disease symptoms. Additionally, serotonin activates both the vagus nerve and gut motility.
Management
As the gut influences the mind, it is rational to emphasize the role of diet in the management of depression. One way of maintaining the integrity of the gut environment involves the intelligent consumption of Polyunsaturated fatty acids (PUFAs). PUFAs share a relationship with both the gut microbiome and our mood. Interestingly, PUFA balance plays an essential role in the sticking of bacteria on gut mucus membrane. Omega-6 PUFA produces molecules that maintain gut mucosal permeability and protect against damage from inflammation.
Bifidobacterium, capable of degrading PUFAs, are less in number in clinically depressed individuals. Fascinatingly, probiotics containing gut-friendly live microbes, show antidepressant effects. Bifidobacterium longum, Lactobacillus casei, and Lactobacillus rhamnosus in probiotics help mend the gut microbial diversity and also elevate anxiety and depression-like behaviours. Faecal microbiota transplant is indeed another promising option in correcting depression.
Taken together
Depression and gut flora are entwined. So, to have an idea of the real situation of your gut, it is crucial to have a ‘Gut Microbiome Test’ done. Latest ‘DNA sequencing technology’ and algorithm-based data acquisition aids in identifying the individualized microbiome signature in the stool samples. Based on the results, a treatment plan consisting of a blend of diet, lifestyle habits, and probiotics are articulated. The resultant lifestyle can help you lead a depression free life.